Surrendering small freedoms is a slippery slope to tyranny.
Category: Opinion
Life, Liberty and the Pursuit of Happiness
Abraham Lincoln, possibly the greatest and most beloved president in the history of the United States, said, “Republicans are for both the man and the dollar, but in case of conflict the man before the dollar.”
Moving the Goalposts — Four Reasons it is Safe to Open America
By Jonathan Geach, M.D.
This article is reprinted from the Conejo Guardian.
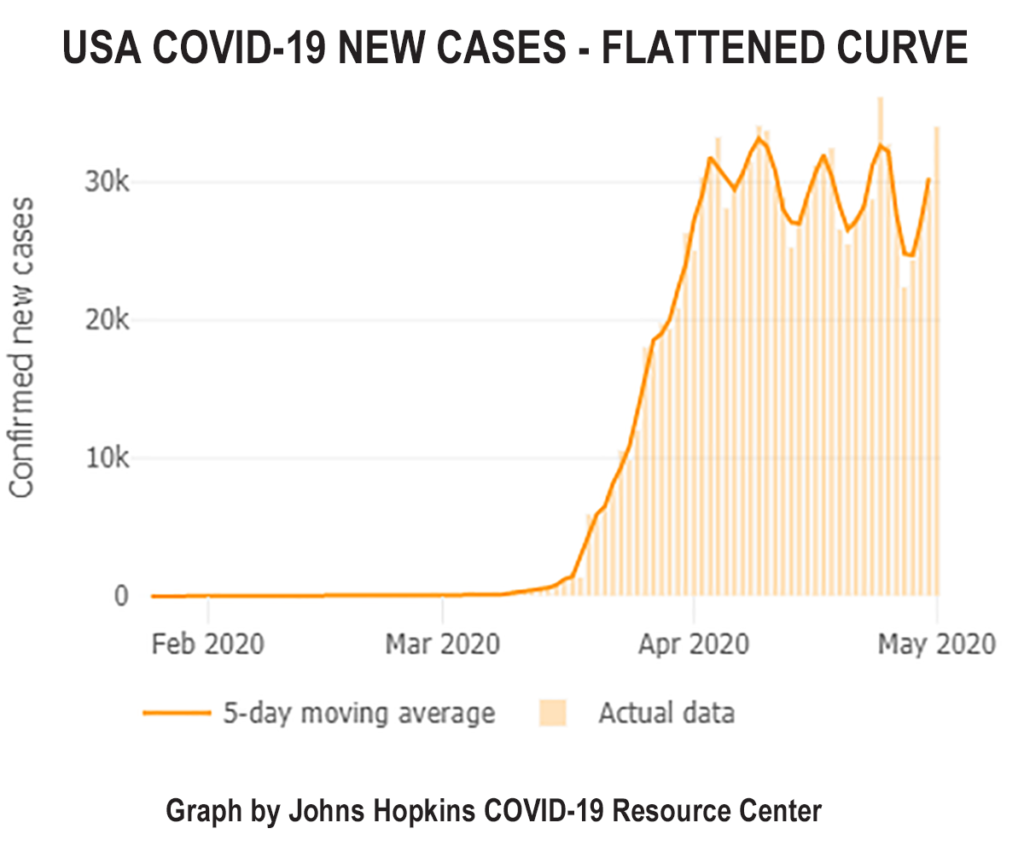
Original Goal: Flatten the Curve
The curve of new infections is declining and we do not need to wait for additional testing or a surveillance apparatus to be in place to reopen America.
In response to warnings that millions of Americans could die, and the carnage COVID-19 created in Italy, state and local governments instituted drastic social distancing in America. In the meantime, the epidemiological curve in the US has followed the trend seen in Europe and is well past its peak.
The Institute for Health Metrics and Evaluation (IHME) model estimates that the peak of deaths in the U.S. occurred on April 13, 2020. This would seem to indicate the time to loosen social distancing and allow a return-to-work has arrived.
Despite this new information, several public health officials have said that May 1 may be too soon to reopen. They claim that we don’t know enough about the virus, and it won’t be safe to reopen America until we have improved testing and surveillance.
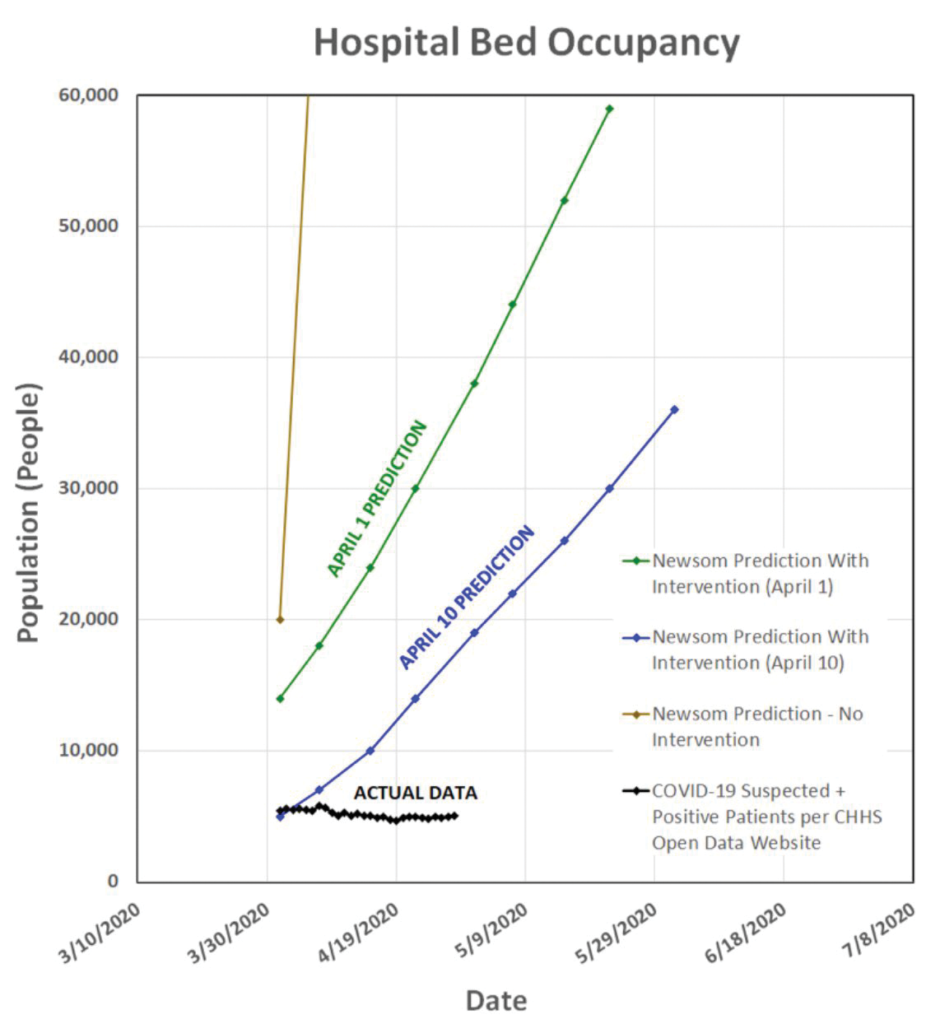
Original Goal: Prevent Healthcare System Saturation
The healthcare system is not overwhelmed, it is underwhelmed and being damaged.
The purpose of “Flatten the Curve” was to prevent the healthcare system from being overwhelmed with patients suffering from COVID-19. The reality is that the healthcare system is now underwhelmed and healthcare workers are being laid off and furloughed in droves as a result of healthcare centers having neglected patient care not related to COVID-19 in fear of a COVID-19 surge that failed to materialize on a nationwide basis. This means tens of millions of patients are failing to receive the medical care they need in a timely manner. Almost every hospital outside of the hotspots is empty.
The dramatic reduction in healthcare utilization and capacity is by no means limited to small, country hospitals. Mayo Clinic is empty: 65% of the hospital beds at Mayo Clinic are empty, as are 75% of the operating rooms. This is the world’s premier medical center. If Mayo Clinic is empty, imagine how dire the situation is at smaller, community-based healthcare centers. Given the complexity of the patients referred to Mayo Clinic, its emptiness alone will have a significant negative impact on healthcare outcomes.
Healthcare underutilization leads not only to patient care being delayed, which will likely result in deaths from delayed cancer diagnoses; it also leads to the loss of countless jobs in the healthcare industry, many of which will never return. Even if the patients that are not being seen at this time are seen several months in the future, many will still suffer negative health outcomes. In Medicine, timing is of the essence and diagnosing and treating a patient today is more beneficial than diagnosing and treating the same patient for the same condition in the future.
If the goal of the shutdown was to flatten the curve and prevent healthcare system utilization, why are we still under a shutdown when the healthcare system is significantly underutilized and tens of thousands of healthcare workers are being terminated or furloughed? Why are we still denying non-COVID-19 patients the care they need when hospitals are sitting idle and laying off staff in droves? The only surge we’ve seen thus far is with respect to initial weekly jobless claims; tragically, there’s a good chance we will see a surge in suicides later this year as well.
Original Goal: Determine the true mortality
The evidence that the true mortality is much lower than early estimates continues to mount.
Now, I know many people will say, “But look at New York. Look at how the hospitals were full and we almost ran out of ICU beds and ventilators. COVID-19 is nothing like the flu.” To these objections I must point out that COVID-19 kills people through a prolonged process that generally keeps people in an ICU on a ventilator for two weeks before they die. Most people who die of the flu have a much faster disease process.
A new study in The New England Journal of Medicine supports the claim that COVID-19 is much more common and mild than first believed. Researchers from Columbia University in Manhattan tested every woman who presented in labor for COVID-19 from March 22 until April 4. Fifteen percent of the women tested positive for COVID-19, but, of these, eighty eight percent were totally asymptomatic. Also interesting, none of the women who tested positive were even sick enough to seek COVID-19 care; they simply came to the hospital to have a baby. Eighty-eight percent of positive women were asymptomatic.
The USS Theodore Roosevelt has been in the news for an outbreak aboard the ship. The US Navy is testing every sailor on board. Of the 4,800 sailors, 600 tested positive and 60 percent of those were entirely asymptomatic.
The first prevalence antibody study from Stanford was released on 4/17/20. After sampling the blood from 3,300 people, researchers found that 48,000 to 81,000 people in Santa Clara county had been previously infected. Only 1000 people tested positive in the county.
Many people are actually claiming that the large number of asymptomatic people with the disease requires prolongation of the shutdowns. The large asymptomatic group does quite the opposite. It demonstrates that the number of people who have already had the disease is very high and the actual infection mortality rate is much lower than we previously believed.
Original Goal: Prevent a catastrophic second wave
If there is a second wave, it will most likely be this fall which will give us plenty of time to prepare
The biggest concern voiced by public officials is that opening the economy is unsafe because it could, “Pour gasoline on the fire.” These officials don’t understand that most people who recovered from the infection are now immune and, thus, contribute to the development of “herd immunity.” If the next wave comes, the peak will be lower or, like in South Korea, where social distancing was only voluntary, it may be just a period of a low rate of new cases until herd immunity is build.
If the current level of herd immunity is so low that a second wave builds, it will take at least several months. The CDC estimated that it will likely be at least 150 days before a possible second wave. This would push it back to the fall at the earliest. A study published in The Lancet also states it would be several months before a possible second wave.
Personal protection equipment (PPE), testing, and surveillance may not be optimized today, but all should be in place by this fall. At that time, politicians and scientists can determine how the elderly and vulnerable can be protected without needing to interrupt the economy.
In addition, the shutdowns are slowing if not preventing the development of herd immunity. This increases the chance and possible severity of a second wave of COVID-19 several months after the shutdowns are lifted.
The idea of herd immunity is simple: Once enough people in society are immune to a disease, if one person becomes infected, the chance they give it to someone else is less than one. It is estimated that 80% of the population would need to be immune to have true herd immunity. However, if we have even half that, we would slow the increase of the virus dramatically. This would make surveillance easier and decrease the chance that a second wave could overwhelm our health care system this fall.
In Summary
Continued shutdowns threaten our economy, our health and even our healthcare system.
The state of our economy is not just a monetary risk, it is a health risk. When people lose their jobs, they typically lose their health insurance. The British Journal of Psychiatry found that there were more than 10,000 “economic suicides” as a result of the 2008 recession. Similarly, a 2016 study from The Lancet found that there were an excess 260,000 cancer deaths as a result of the recession. These statistics also fail to mention the increased domestic violence, increased child abuse and home loss when schools and businesses are closed.
In spite of the moving goalposts: The number of new cases is declining. The mortality is likely much lower than early estimates. Those who have been infected by the disease will most likely be immune for at least a year. Finally, the lives saved by starting the economy sooner vastly outnumber those that could be saved by extended shutdowns.
Contributors:
Jonathan Geach, M.D.
Ankur J. Patel, M.D.
Knut M. Wittkowski, PhD, ScD
Lacy Windham, M.D.
Ashkan Attaran, M.D.
Jason Friday, M.D.




